Introduction
Mammography is the routine method for breast cancer screening. This modality is able to elicit calcifications inside breast tissue. These calcifications can be seen in two general forms including micro-calcification and macro-calcification. Macro-calcification is usually associated with benign lesions, while micro-calcification is associated with neoplastic lesions [1]. Another imaging finding seen in mammography is the calcification of breast arteries (or breast arterial calcification – BAC). This finding is regarded as a normal phenomenon in elderly post-menopausal women [2]. BACs are radio-opaque linear lesions that are not situated near the areola [3]. Descriptive studies have shown that BACs are commonly seen in elderly women with stablished risk factors for arteriosclerosis. Unlike typical arteriosclerotic lesions, calcium is deposited in the media of the arteries, instead of the endothelium. Early observational studies have been able to detect a link between the existence of BAC and calcification of coronary arteries, which is diagnosed by computed tomography (CT)-angiography and is shown to be significantly associated with increased cardiovascular diseases [4], although these observations have been challenged by case-control and cross-sectional studies in which there has been no significant relation between BAC and coronary calcification. BAC in particular has also been directly linked with an increased risk of acute myocardial infarction, although observations have not yielded consistent results [5]. Because of the regularity with which mammography is performed, especially in developed nations, and the possible predictable role of BAC in cardiovascular disease, some have suggested that mammography could be used as a surrogate screening method for cardiovascular diseases. But this desire is not limited to academic scholars, as a study performed by Margolies et al. suggested that patients would also prefer to be notified about possible cardiovascular diseases using BAC estimation [6]. In the present study we aim to assess the relation between BAC and coronary calcium score, and also the association of BAC with risk factors of cardiovascular diseases.
Material and methods
Patients
The present cross-sectional study was performed in a tertiary medical centre, which was a referral centre for cardiovascular diseases. This study included 60 patients who were referred to undergo CT-angiography. Inclusion criteria consisted of being referred to our centre with a diagnosis of coronary artery disease by a cardiologist. Exclusion criteria consisted of having a past medical history of breast cancer and not wanting to participate in the study.
Sample size calculation
Sample size was calculated by the following formula:
Power = 80%, a = 0.5 → Za = 1.96, β = 0.8 → Zb = 0.842, C = 0.5 * ln [(1 + r)/(1 – r), N = [(Za + Zb)/C]2 + 3 = 53. In this study, 60 patients were included.
Calcium scoring
Calcium scoring was performed according to the latest guideline published by the cardiac society of Australia and New Zealand [7]. Calcium score was calculated by determining the area of calcification and multiplying it to the highest Hounsfield unit. Calcium score was classified into five sets of values, equalling zero, between 1 and 10, between 11 and 100, between 101 and 400, and more than 400. To determine this score, a 64-slice CT-angiography machine (Siemens, Germany) was used.
Breast artery calcification evaluation
BAC is evaluated by determining the density, number, and length of calcified vessels. Each of these parameters are attributed a score, and the sum of these determines the BAC value. BAC values are categorised into three subgroups, BAC equalling zero, between 1 and 6, and between 7 and 12. In this study, we used a simpler method for BAC classification. Mild BAC was defined as scant calcification in vessels, in which the distance between the calcifications was at least 10 cm. Moderate BAC was defined as the calcification of the complete length of an artery, and sever BAC was defined as having complete calcification in multiple arteries.
Mammographies were obtained using the Hologic Dimension unit (Bedford, MA, USA).
Results
The mean age of patients included in the study was 49.52 ± 8.83 years. From all of the patients, 30 had experienced menopause. Only one patient had a history of cigarette smoking. The time period between the CT angiography and the mammography is documented in Table 1. As it can be seen the most common time interval was four months.
Table 1
Time interval between computed tomography (CT)-angiography and mammography in patients
| Time interval between CT-angiography and mammography (months) | n (%) |
|---|---|
| 2 | 7 (11.7) |
| 3 | 8 (13.3) |
| 4 | 20 (33.3) |
| 5 | 16 (26.7) |
| 6 | 9 (15) |
Table 2 depicts the calcium scores and BAC values documented for the patients. Of all the patients, 37 had evidence of calcification in their coronary arteries and 50 patients had evidence of breast artery calcification. Paired t-test showed that there was a significant relation between having coronary calcification and breast artery calcification (p = 0.001).
Table 2
Calcium scores and breast artery scores of patients included in the study
| Calcium score | BAC grades | Total | |||
|---|---|---|---|---|---|
| None | Mild | Moderate | Severe | ||
| 0 | 7 | 16 | 0 | 0 | 23 |
| 1 | 2 | 13 | 0 | 0 | 15 |
| 2 | 1 | 9 | 4 | 0 | 14 |
| 3 | 0 | 1 | 4 | 1 | 6 |
| 4 | 0 | 0 | 1 | 1 | 2 |
| Total | 10 | 39 | 9 | 2 | 60 |
There was no significant relation between menopausal women and those with ongoing ovulatory cycles regarding the existence of calcified coronary or breast arteries. There was a significant relation between the existence of risk factors such as diabetes, hypertension, and hyperlipidaemia and calcified breast and coronary arteries (p < 0.0001).
The relation between the severity of calcification of the breast arteries and the coronary arteries was also determined. There was a significant relation between the increase in one value and the increase in the other (p < 0.001).
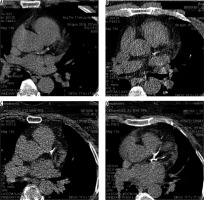
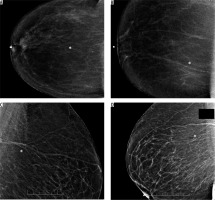
Figure 1 is a schematic presentation of breast artery calcification staging. Figure 2 demonstrates selected coronary calcification depictions of the patients included in the study. Figure 3 shows breast artery calcification in selected patients who were included in the study.
Figure 1
Schematic presentation of breast arterial calcification. The figures indicate increasing grade from A to D. The grading is done based on severity and density of calcium deposition in breast arteries

Discussion
There has long been a discussion regarding the clinical significance of calcification of the media of the arteries, and its compression to intimal calcification. Although it has been known that medial thickening of the artery is associated with high blood pressure, not much is known about how medial thickness contributes to coronary heart disease, or whether it is related with intimal calcification, which is proven to be associated with cardiovascular disease [8]. Importantly, observational studies have reported that similar risk factors exist for intimal and medial thickness and calcification [9]. Because of these links between the two types of calcification, it is hypothesised that vascular calcifications of both kinds could be related and be of prognostic and diagnostic value towards each other.
Mammography is currently the main method of breast cancer screening in women over 40 years old, and guidelines suggest annual imaging after a certain age, with the exact age cut-off still a controversy [10]. Mammography is able to show breast artery calcification of medial type, and could be associated with intimal thickness in coronary arteries, which is shown to be an aetiopathological starting point for the progression of coronary artery disease, the main cause of global burden of disease [11].
An early study performed by Henkin et al. studied the relation between BAC and coronary artery disease proven by angiography on 319 patients aged between 50 and 70 years but did not find an association. The patients with coronary artery disease had an increased prevalence of risk factors for ischaemic heart disease, and a marginally increased rate of BAC, but the difference between the two groups was not significant. They found that the existence of hypertension and being aged above 63 years were significantly related to the existence of BAC [12]. This finding could be of significance, knowing that most breast cancer screening programs continue until the age of 63 years, but most not much further [13]. Another study performed by Pecchi et al. found that BAC was associated with coronary artery disease in a group of post-menopausal women, a group of patients with a higher mean age [14]. Penugonda et al. suggested that BAC did not even correlate with risk factors associated with coronary artery disease, and that it was not significantly related with symptomatic coronary disease. They even suggested that patients with BAC had lower prevalence of myocardial infarction, compared to those without BAC [15]. Moradi et al. conducted a similar study and found similar results [16]. Matsumura et al. found the exact opposite in asymptomatic women – they found that patients with BAC had an odds ratio of over 22 to have calcium scores more than 400. This association was not witnessed in patients with calcium scores of 0, suggesting that the absence of BAC is not as suggestive of a coronary condition as its existence [17]. Again, this negative predicting role may be of significance in elder populations, though no study has focused on this issue so far.
Another issue which is suggested to play a role in the relation between CAD and BAC is race; all of the previously mentioned articles were performed on Caucasian populations. Newallo et al. studied a group consisting of African American women with a median age of 52.5 years. In the 204 patients included, 42 had BAC in mammography. There was a significant relation between the existence of BAC and calcium scores of more than 100, luminal narrowing, and stenosis of over 50% of coronary vessels [18].
Calcium scores of over 400 are usually found to be clinically significant, but low levels of calcium score, even as low as 10, are found to be associated with increased risk of cardiovascular accidents. A study by Chadashvili et al. showed that BAC correlated with calcium scores of more than 11. BAC in particular was related with cardiovascular risk factors, such as diabetes and renal disease [19]. Fanthala et al. reported similar results in a retrospective study performed on 307 Arab women [20].
A recent large-scale cohort study performed on 5145 people aged between 60-79 years and of different ethnicities was performed to assess the relation between BAC and cardiovascular diseases and risk factors. It was found that as age increased, the probability of finding BAC also increased (19% in women aged between 60 and 64 years compared to 52% in those aged 75-79 years). The intensity of BAC also increased with age. BAC was more common in Hispanic populations, followed by Caucasians, Blacks, and Asians. The first publication from this study focuses on the recruitment characteristics, and future publications will guide clinicians and researchers in better understanding the predictive role of BAC in cardiovascular diseases [21].
A recent review on the possible applications of BAC in cardiovascular disease risk stratification proposed that, although the concept of using BAC for CVD was appealing, there were major barriers to overcome. One barrier was the technical heterogeneity in which the measurements are made, and also the different cut-off values defined for increased calcium score values (as seen before, different scholars have used values ranging from 10 to more than 400 to define a clinically significant positive calcium score). Another noteworthy limitation is how the progress of imaging techniques has affected BAC detection. Interestingly, newer studies tend to better detect BAC and Coronary artery disease, making old evidence less relevant, and dictating the need for more studies performed with the latest appliances available [22]. One novel aspect of technology recently applied in this regard is deep learning algorithms, which have been able to detect BACs as well as expert radiologists, and may be a significant contribution to systemic screening of women for both breast anomalies and cardiovascular diseases [23].
Altogether, compelling evidence exists to support the use of BAC in clinical practice, but there is not enough evidence to support how and to what extent BAC should be used as a risk factor for coronary artery disease, and most importantly ischaemic heart disease. Larger scale cohort studies will be of merit in this regard. Further technical notes will also be needed to formulate a standardised method for imaging of BAC and applying it in clinical contexts.
Conclusions
BAC was significantly related to the existence of coronary artery calcification detected in CT-angiography. This relation is not affected by age. BAC was also associated with an increased prevalence of coronary artery disease risk factors, such as diabetes, hyperlipidaemia, and hyper-tension.